Photoimmunotherapy (PIT) busts open the doors for drug delivery
Photoimmunotherapy (PIT) busts open the doors for drug delivery
Ken Tichauer
Over the last decade alone, it is estimated that over $200 billion has been spent just by governments to fund cancer research [1]. Despite this enormous investment, the recently released 2014 World Heath Organization (WHO) Cancer Report suggests that cancer incidence rates and deaths from cancer are on the rise, both in more developed and less developed nations.
Many now believe that the paucity of significant advances in cancer therapy stem from two salient factors in cancer biology:
1) Every tumor is genetically unique, with more aggressive forms exhibiting multiple genetic variants within a single tumor. This means that even sophisticated new therapies that can target specific molecules associated with cancer cells, are ineffective at killing all cancer cells in a patient.
2) Poorly formed vasculature and high tissue pressures in tumors can make it difficult for systemically delivered drugs to reach all areas of a tumor.
These factors mean that some cells will inevitably be resistant to any conventional therapies, and when these cells regrow, the recurring disease is increasingly resistant to available therapies.
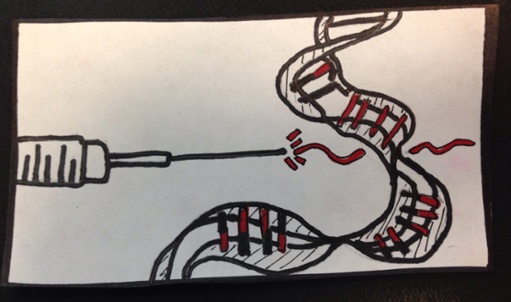
As chief scientist in the Molecular Imaging Program at the National Cancer Institute in Bethesda, MD, Professor Hisataka Kobayashi, MD PhD, and his group have recently developed an exciting new paradigm for cancer therapy that appears to tackle both of the major hurdles. They have proposed to combine two forms a cancer therapy in succession. The first is a new approach developed in their lab that they have coined, “Photoimmunotherapy” (PIT). PIT entails injecting a photosensitive agent that is targeted to a key cell surface molecule overexpressed in an individual’s cancer. The characteristics of these drugs are such that it is non-toxic until it is both attached to a cancer cell and exposed to a light source, which activates the drug resulting in cell death. Since the drug is only targeted to cancer cells, healthy cells are, by-and-large, safe from damage.
Alone, however, PIT would be no more successful than other available molecular-targeted therapies: only the cancer cells that express the particular targeted molecule would be affected, while other genetically different cancer cells within the tumor would be unaffected, resulting in a regrowth of a more drug-resistant tumor. The unique advantage of PIT is that it appears to be able to break down the barriers that make some tumors particularly resistant to conventional chemotherapies, resulting in what Prof. Kobayashi describes as a super EPR (enhanced permeability and retention) effect. In other words, a very large proportion of any therapeutic will accumulate in a cancer if given subsequent to PIT treatment, resulting in a significant magnification of their efficacy. Early studies in mouse studies have demonstrated an incredible ability for this combined therapy to result in a complete killing of even very aggressive and heterogeneous tumors [2].
You can see Prof. Kobayashi speak about this exciting project and more at the upcoming Biomed 2014, where he will expand on new clinical trials he is proposing to explore the full potential of this promising new approach to cancer therapy.
[1] S. Eckhouse, G. Lewison, and R. Sullivan, “Trends in the global funding and activity of cancer research,” Mol Oncol, 2(1), 20-32 (2008).
[2] H. Kobayashi, R. Watanabe, and P. L. Choyke, “Improving Conventional Enhanced Permeability and Retention (EPR) Effects; What Is the Appropriate Target?,” Theranostics, 4(1), 81-89 (2013).