An Eye on the Future of Vision
An Eye on the Future of Vision
Rebecca Andersen
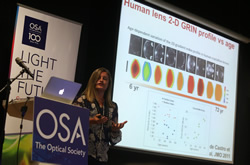
Dr. Susana Marcos, Professor of Research Instituto de Optica, Consejo Superior de Investigaciones Científicas, Madrid, Spain

The eye is a fascinating optical system, yet its performance gets compromised with age and disease. Marcos' presentation detailed the future of ophthalmology.

Susana Marcos with Eric Van Stryland, OSA Fellow and 2006 president of The Optical Society.
In only 25 years, this non-invasive imaging technology has become a well-established fixture in the medical offices of ophthalmologists. While the OCT imaging continues to develop, novel techniques and new swept-source systems are reducing the cost of OCT platforms. Susana Marcos has pioneered research in novel imaging techniques to assess the optical properties of the ocular optics and the human retina. These imaging techniques are addressing the growing needs of the aging population around the world.
“Around the world a billion people worldwide suffer from poor vision because they do not have the prescription eyeglasses they need. For these people, a low-cost pair of eyeglasses would greatly improve their access to education, productivity, and overall quality of life,” stated Marcos. “Unfortunately, there is an acute shortage of trained optometrists to prescribe eyeglasses in low-resource settings. In the U.S., there is one optometrist to every 6,000 people. In India, this number jumps to one optometrist to every 250,000 people. In addition to the limited number of optometrists globally, not all of these physicians have the most current tools available for measuring a prescription.”
What is the future of refractive correction in vision?
Marcos detailed specialized advancements such as – electroactive glasses, customized LASIK and chip implanted contact lenses. What will help to enable this future? We will see advancements in hand-held OCT imagining and the ability for optometrists to more easily to take automatic and more accurate assessments of their patients.
In the last decade, lens companies have designed intraocular lenses that not only replace the cloudy lens of the eye but can also correct the patient’s vision, to reduce the need for glasses. This correction is not perfect, however. The natural lens is stretched by muscles in the eye to change its shape, and thus its focal length, to shift from having up-close and far objects in sharp focus on the retina. Current implanted intraocular lenses do not have this capability to change shape like this. Instead, standard intraocular lenses are monofocal (i.e., they correct only far vision) which creates sharp vision for far-away objects but blurred vision for objects close by. Patients would then wear glasses to correct near. There are also newer multifocal lenses that focus both near and far objects onto the retina at the same time but with some loss of image quality and contrast for both near and far distances. The choices for monofocal, and, particular multifocal intraocular lenses keeps growing as more designs enter the market.
Taking optics to vision
Today’s adaptive optical technologies are in many ways the core of vision improvements. Using the same adaptive optics that are used in astronomy, we may get to the point where we are able to ask ourselves “what might the world look like if we could see with the eyes of another? Using adaptive optics. We may be able to manipulate the vision of another,” remarked Marcos.
The currently available hand-held, see-through multifocal vision simulator based on temporal multiplexing of a tunable lens. Visual performance and perceptual quality with multifocal corrections then varies across patients, although they were more uniform across distances than monofocal corrections. The simultaneous vision simulator proved a promising compact tool to study visual performance with multifocal corrections and to select the lens design best suited for each patient, alternative to costly and bulky adaptive optics based devices.
Restoring Eyesight in the Future
The restoration of vision will be achieved in the future by creating devices, retinal prostheses, that receive and process incoming light and then transmit the information in the form of electrical impulses to the remaining inner retinal layers for visual function. The image captured in the camera is then sent to the brain for interpretation.
Ophthalmology research and the advancement of vision will only continue through the use of optics and photonics. A cure for presbyopia is one of ophthalmology’s holy grails, but until the cure arrives, helping patients manage it is the name of the game for Marcos and her team.
